
Impact of Multiple Chronic Conditions on Activity Limitations Among Older Mexican-American Care Recipients
ORIGINAL RESEARCH — Volume 15 — May 3, 2018
Diane M. Collins, OT, PhD1,2; Brian Downer, PhD2; Amit Kumar, PhD, MPH3; Shilpa Krishnan, PT, PhD4; Chih-ying Li, PhD1; Kyriakos S. Markides, PhD5; Amol M. Karmarkar, PhD, MPH2 (View author affiliations)
Suggested citation for this article: Collins DM, Downer B, Kumar A, Krishnan S, Li C, Markides KS, et al. Impact of Multiple Chronic Conditions on Activity Limitations Among Older Mexican-American Care Recipients. Prev Chronic Dis 2018;15:170358. DOI: http://dx.doi.org/10.5888/pcd15.170358.
PEER REVIEWED
Abstract
Introduction
Older Mexican Americans are living longer with multiple chronic conditions (MCCs). This has placed greater demands on caregivers to assist with basic activities of daily living (ADL) or instrumental activities of daily living (IADL). To understand the needs of older Mexican-American care recipients, we examined the impact of MCC on ADL and IADL limitations.
Methods
We analyzed data from 485 Mexican American care-receiving/caregiving dyads. Selected MCCs in the analysis were diabetes, hypertension, stroke, heart disease, arthritis, emphysema/chronic obstructive pulmonary disease, cognitive impairment, depression, and cancer. Care recipients were dichotomized as having 3 or more conditions or as having 2 or fewer conditions. Three comorbidity clusters were established on the basis of the most prevalent health conditions among participants with comorbid arthritis and hypertension. These clusters included arthritis and hypertension plus: diabetes (cluster 1), cognitive impairment (cluster 2), and heart disease (cluster 3).
Results
Care recipients with 3 or more chronic conditions (n = 314) had higher odds of having mobility limitations (OR = 1.98; 95% CI, 1.34–2.94), self-care limitations (OR = 2.53; 95% CI, 1.70–3.81), >3 ADL limitations (OR = 2.00; 95% CI, 1.28–3.17), and >3 IADL limitations (OR = 1.88; 95% CI, 1.26–2.81). All clusters had increased odds of ADL and severe ADL limitations. Of care recipients in cluster 2, those with arthritis, hypertension, and cognitive impairment had significantly higher odds of mobility limitations (OR = 2.33; 95% CI, 1.05–5.24) than those with just arthritis and hypertension.
Conclusion
MCCs were associated with more ADL and IADL limitations among care recipients, especially for those with hypertension and arthritis plus diabetes, cognitive impairment, or heart disease. These findings can assist in developing programs to meet the needs of older Mexican-American care recipients.
Introduction
Older adults residing in the United States are projected to become more racially and ethnically diverse in the next 40 years. The Hispanic population is the largest minority group, comprising 17.6% of the total US population (1). The Hispanic population aged 65 years or older numbers 3.1 million and is anticipated to reach 15.4 million by 2050 (2).
Mexican Americans are the largest Hispanic population in the United States (3). On average, older Mexican Americans are socioeconomically disadvantaged and are more likely than non-Hispanic whites to have chronic health conditions, including osteoarthritis, diabetes, hypertension, stroke, and cognitive decline (4,5). Despite these socioeconomic and health disadvantages, Hispanics have a longer life expectancy than non-Hispanic whites, which is called the Hispanic Paradox (6). This paradox is greatest among foreign-born Mexican Americans; because of their self-selection, individuals born in Mexico who migrate to the United States tend to have better health characteristics than those who stay in Mexico. This positive health selection may in part contribute to lower mortality rates for foreign-born Mexican Americans than their African American and white counterparts because of heart disease, smoking, and other causes (6,7).
Familismo, a cultural practice of many Hispanics, refers to emotional attachment and strong sense of loyalty and solidarity among family members (8). This practice contributes to older Hispanics being less likely than non-Hispanic whites to use formal health care services such as nursing homes, long-term care, or home health services (9–11). Hence, they place increased demands on their family members for routine and complex tasks.
Aging predisposes people to a high risk of developing multiple chronic conditions (MCCs) (12). Many studies identified combinations of multiple chronic conditions (13–17) and examined their impact on activities of daily living (ADL) and instrumental activities of daily living (IADL) limitations among older adults (18,19). Studying the relationship between multiple chronic conditions and the functional characteristics of older Mexican Americans is important given this population’s long life expectancy, high prevalence of chronic health conditions, and dependence on family care. An understanding of the impact of multiple chronic conditions on assistance needs among older Mexican Americans is crucial to plan appropriate health care delivery.
The objective of this analysis was to examine the impact of multiple chronic conditions on the ADL and IADL limitations of older Mexican Americans. We also explored potential differences in the ADL and IADL limitations of older Mexican Americans with different combinations of multiple chronic conditions.
Methods
Sample population
We used data from the seventh observation wave of the Hispanic Established Populations for the Epidemiologic Study of the Elderly (HEPESE). Detailed descriptions of the sampling procedures and data collection techniques of the HEPESE are provided elsewhere (20). HEPESE is an ongoing longitudinal study of older Mexican American adults living in Texas, New Mexico, Colorado, Arizona, and California. The baseline observation wave (1993–1994) included 3,050 Mexican Americans aged 65 or older; 9 total observations were completed as of 2016. During wave 7 (2010–1011), 1,078 older adults were interviewed, 925 of whom provided contact information for an informant who was the primary person they would go to for advice or help with things they are unable to do by themselves. The informant reported characteristics of the respondent (eg, health, financial status, functional abilities) and provided information on assistance required by the respondent to complete ADLs and IADLs. The institutional review board at the University of Texas Medical Branch approved the HEPESE study before data were collected.
Because this study focused on care recipients who needed assistance from caregivers to complete self-care and household tasks, respondents who reported they were independent in self-care and household tasks (n = 329) were excluded from this study. Studies using data from the HEPESE used a similar approach to selecting study care recipients who needed assistance (21). Fifty-seven care recipients were also excluded from the sample because they did not receive the Mini Mental Status Exam, and 54 care recipients were excluded because of missing information for sociodemographic or health characteristics. Thus, 485 care-recipient/caregiver dyads comprised the final sample (Figure).
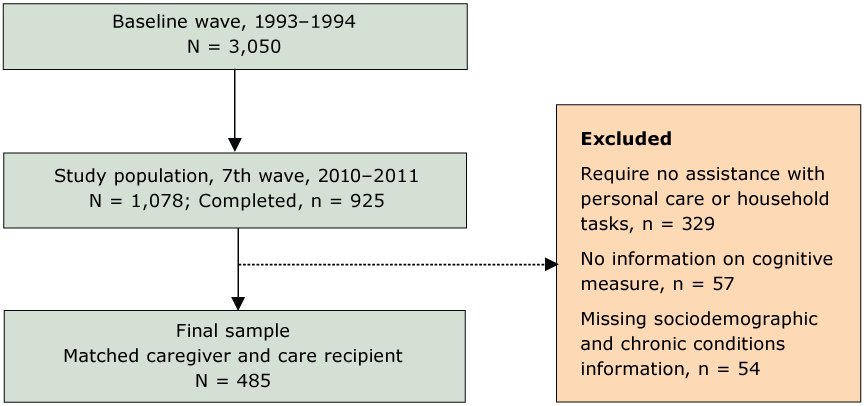
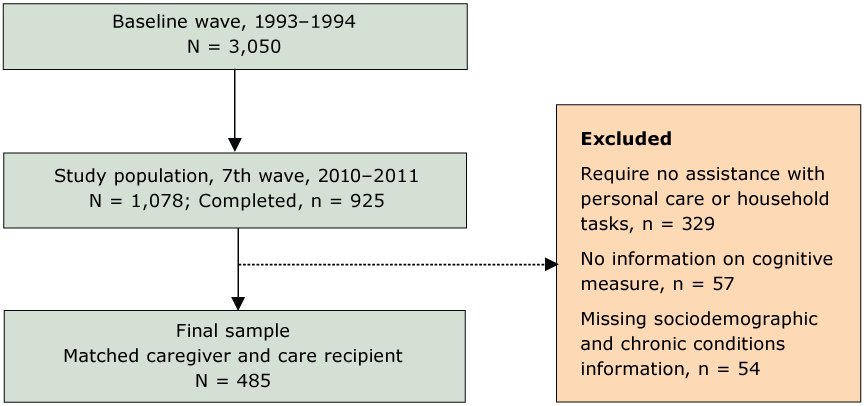
Figure.
Flowchart showing exclusion criteria for study on effect of multiple chronic conditions on activity limitations among Mexican Americans, Hispanic Established Population for the Epidemiologic Study of the Elderly, 2010–2011. [A text description of this figure is available.]
Flowchart showing exclusion criteria for study on effect of multiple chronic conditions on activity limitations among Mexican Americans, Hispanic Established Population for the Epidemiologic Study of the Elderly, 2010–2011. [A text description of this figure is available.]
Measures
Sociodemographic measures collected from the care recipients were age, sex, years of education completed, and marital status (married, widowed, not married). Chronic conditions consisted of diabetes, hypertension, stroke, heart disease, arthritis, emphysema/chronic obstructive pulmonary disease, cognitive impairment, high depressive symptoms, and cancer. These health conditions were selected on the basis of previous literature (13–15,18,19) and health conditions included in the HEPESE questionnaire. These conditions, with the exception of depression and cognitive impairment, were identified based on self-report of the care recipient. Care recipients with a systolic blood pressure of 140 mm Hg or higher, or a diastolic blood pressure of 90 mm Hg or higher were also classified as having hypertension. Care recipients with high depressive symptoms were identified by a score of 16 points or higher on the Center for Epidemiologic Studies Depression (CESD) Scale (22). Cognitive impairment was defined as scoring 17 points or lower on the Mini Mental Status Exam (23).
Multiple chronic conditions is commonly defined as the presence of 2 or more health conditions (24). Preliminary analysis of the 485 care recipients included in the final sample indicated that 73 (15.1%) had fewer than 2 chronic conditions and only 15 (3.1%) had no chronic conditions. In the United States, adults with 3 or more chronic conditions make up only 28% of the total population but contribute to 67% of total health care expenditures (25). On the basis of findings from our preliminary analysis, we divided care recipients into 2 groups: those with 2 or fewer chronic conditions (reference group) or those with 3 or more chronic conditions.
We also identified 3 comorbidity clusters to investigate whether ADL and IADL limitations of care recipients varied according to the prevalence of individual combinations of chronic health conditions. The comorbidity clusters were created by using a multistep process. First, we identified the 2 most common health conditions among care recipients in the final sample. Consistent with research, arthritis and hypertension were the most common (18,26). Next, we identified care recipients who had comorbid arthritis and hypertension (n = 281). Finally, we identified the 3 most common health conditions among the 281 care recipients with comorbid arthritis and hypertension. This resulted in the three comorbidity clusters, which were arthritis and hypertension plus: diabetes (Cluster 1; n = 132), cognitive impairment (Cluster 2; n = 90), and heart disease (Cluster 3; n = 111). These comorbidity clusters were analyzed separately, because some care recipients could be included in more than one cluster. For example, a care recipient with arthritis, hypertension, diabetes, and heart disease would be included in Cluster 1 and Cluster 2.
Interviewers asked caregivers if the care recipient required assistance from a person (either the caregiver or another person), special equipment, or both, to complete ADL and IADL. ADL included walking across a small room, bathing, grooming, dressing, eating, getting from a bed to a chair, and using the toilet. IADLs included using a telephone, driving a vehicle or traveling alone, shopping, preparing a meal, doing light housework, taking medication, and managing finances. ADL items were grouped into mobility tasks (walking across a small room, getting from a bed to a chair) and self-care tasks (bathing, grooming, dressing, and eating). Severe ADL limitations and severe IADL limitations were defined as being unable to complete more than 3 ADLs and more than 3 IADLs, respectively.
Statistical analysis
We used analysis of variance and χ2 statistical tests to compare the sociodemographic and health characteristics of care recipients with 3 or more health conditions to those with 2 or fewer health conditions. We conducted multivariable logistic regression models to estimate the odds of care recipients having limitations in one or more mobility tasks or self-care tasks, severe ADL limitations, and severe IADL limitations, according to the 3 comorbidity clusters. All analyses adjusted for the age, sex, education, and marital status of the care recipient. All statistical analyses were performed using R, version 3.1.0 (R Foundation) (27).
Results
Overall, the mean age of the care recipients was 86.2 years, 66% were female, and the mean years of education completed was 4.5 years (Table 1). Arthritis and hypertension were both present in most care recipients. Diabetes, cognitive impairment, and heart disease were observed for approximately 30% of care recipients. Approximately 10% of care recipients reported having had a stroke or having been diagnosed with emphysema/chronic obstructive pulmonary disease (COPD) or cancer. Compared with care recipients with 2 or fewer health conditions, those with 3 or more health conditions were more likely to be female, completed fewer years of education, and were less likely to be married (Table 1).
Fifteen care recipients (3.4%) had zero health conditions and 92 (19.0%) had 5 or more health conditions (Table 1). Of all care recipients, 314 (64.7%) had 3 or more chronic conditions. Hypertension, arthritis, and diabetes (Cluster 1) were present in 132 care recipients; 90 had hypertension, arthritis, and cognitive impairment (Cluster 2); and 111 had hypertension, arthritis, and heart disease (Cluster 3). A total of 253 care recipients had limitations for mobility tasks, 255 had limitations for self-care tasks, 153 had severe ADL impairment, and 280 had severe IADL impairment.
Of total study participants (N = 485), 171 (35.3%) had 2 or fewer chronic health conditions, and 314 (64.7%) had 3 or more chronic health conditions (Table 1). The 2 groups did not differ significantly in age, but did differ in the remaining variables, including sex, education, marital status, and presence of the following health conditions: diabetes, hypertension, arthritis, stroke, heart disease, high depressive symptoms, cognitive impairment, emphysema/COPD, and cancer. Those in the 3 or more chronic health conditions were more likely to have limitations in ADL and IADL. Compared with care recipients with 2 or fewer health conditions, those with 3 or more were more likely to be female, to have completed fewer years of education, and were less likely to be married.
Results of the multivariable logistic regression indicated that care recipients with 3 or more chronic conditions had significantly higher odds compared with care recipients with 2 or fewer chronic conditions of having limitations in one or more mobility tasks (odds ratio [OR] = 1.98; 95% confidence interval [CI], 1.34–2.94), self-care tasks (OR = 2.53; 95% CI, 1.70–3.81), and to have severe ADL limitations (OR = 2.00; 95% CI, 1.28–3.17) and severe IADL limitations (OR = 1.88; 95% CI, 1.26–2.81) (Table 2). Among the 3 comorbidity clusters, cluster 2 (arthritis, hypertension, cognitive impairment) was the only cluster associated with significantly higher odds of limitations in one or more mobility tasks (OR = 2.33; 95% CI, 1.05–5.24). All 3 comorbidity clusters were associated with increased odds of limitations in self-care tasks, severe ADL limitations, and severe IADL limitations. Comorbidity cluster 3 (arthritis, hypertension, heart disease) was associated with the highest odds of limitations in self-care tasks (OR = 5.67; 95% CI, 2.57–13.00), whereas comorbidity cluster 2 (arthritis, hypertension, cognitive impairment) was associated with the highest odds of severe ADL limitations (OR = 4.51; 95% CI, 1.83–12.41) and severe IADL limitations (OR = 4.36; 95% CI, 1.91–10.25).
Results from the comparative analysis of the 3 comorbidity clusters indicated that only cluster 2 (arthritis, hypertension, cognitive impairment) had a significantly higher chance of needing assistance with mobility tasks. Multiple chronic conditions were associated with more ADL and IADL limitations, especially for care recipients with hypertension and arthritis plus diabetes, cognitive impairment, or heart disease (Table 2).
Discussion
We found that care recipients with 3 or more chronic conditions needed caregiving assistance with mobility, self-care, and ADL- and IADL-related tasks, regardless of their combination of chronic conditions. Studies show that older Mexican Americans often have multiple chronic conditions (28) that can limit their ability to live independently (12). Given a choice, many aging Americans would prefer to stay in their homes and communities rather than be placed in nursing homes, a concept known as “aging in place.” The older Mexican American population is no different in their preferences; however, they tend to rely on family members for their health care needs rather than using local formal health care resources. The use of health care, including hospital stays, physician visits, and costs, increases among adults with multiple chronic conditions (26,29).
Our study showed that all 3 chronic condition clusters were associated with increased odds of limitations in self-care tasks, severe ADL limitations, and severe IADL limitations. Care recipients with arthritis, hypertension and heart disease (cluster 3) were most likely to require assistance with basic self-care tasks. A study reported that unpaid caregivers caring for individuals with heart disease perceived they themselves had difficulty in performing tasks such as household cleaning and management of bills and finances (30). Older adults with cognitive impairment have higher risk of mobility impairment and physical decline (31,32), which can further complicate their care. Furthermore, older adults with cognitive impairment often require supervision to prevent injury even if they are able to perform some self-care or household tasks.
Because older adults are living longer, their informal caregivers will most likely age and experience health problems and functional impairments themselves, which may contribute to greater burden for caregivers. Moreover, caring for older Mexican Americans with multiple chronic conditions, especially those with cognitive impairments, can be challenging. Informal caregivers serving a minority population tend to provide more and higher intensity of care than caregivers serving nonminority populations (33). A previous study determined that caregivers of Mexican Americans who had more involved mobility impairments, limitations in IADLs, depressive symptoms, and cognitive decline were more likely to have psychological distress (21). Similarly, another study found that caregivers of Mexican Americans aged 70 years or older had fewer physician visits than their non-caregiving counterparts (34). Among new caregivers of older Mexican Americans, those who had high levels of acculturation (ie, who have lived in the United States for a longer duration) were more likely to report depressive symptoms at 2 years after the start of caregiving than those with lower levels of acculturation (35).
Our study has limitations. Our sample was restricted to 5 southwestern US states and may not be representative of other growing populations of older Hispanics in other US locations. Our inclusion criteria for this analysis resulted in the most impaired older Mexican Americans being selected, which may have inflated the percentage of the final sample with hypertension, diabetes, and heart disease. This analysis focused on older Mexican Americans who had limitations in daily activities, and we excluded those who did not have limitations in ADLs or IADLs. This exclusion may have influenced our results since older Mexican Americans with multiple chronic conditions, but who did not need assistance in daily activities, were excluded from the final sample. The chronic conditions identified in the HEPESE data set were based on self-report from care recipients and could be subject to recall bias. Furthermore, many chronic health conditions that may affect ADL and IADL functioning (eg, atrial fibrillation, high cholesterol) were not collected in HEPESE. Finally, participants who did not provide contact information for an informant could not be included in our analysis, which may have influenced our results; these participants may not need help from another person and thus may be in better health than participants who did provide information for an informant. Alternatively, participants who did not provide contact information for an informant may have less social support than participants who did provide contact information for an informant.
Our analysis also has strengths. First, the HEPESE is a well-characterized cohort of older Mexican American adults that includes measures for a range of sociodemographic, health, and functional characteristics. Second, data for ADL and IADL limitations of the care recipient were collected from an informant (informal caregiver) who has insight of the functional characteristics and health care conditions of the care recipient.
Many older Mexican-American care recipients are living with multiple chronic conditions. Our analysis provides evidence that older Mexican American care recipients with 3 or more health conditions are highly likely to have severe ADL and IADL limitations and difficulty completing self-care and mobility tasks. Care recipients with comorbid arthritis and hypertension along with diabetes, cognitive impairment, or heart disease may be most likely to have functional limitations. Our findings can ensure that resources are appropriately allocated to caregivers on the basis of physical and cognitive impairments of older Mexican-American care recipients.
Acknowledgments
This work was supported by the National Institute on Aging (NIA) grant no. R01 AG010939. Research reported in this publication was supported by the UTMB Claude D. Pepper Older Americans Independence Center grant P30 AG024832 from the NIA of the National Institutes of Health (NIH). The content is solely the responsibility of the authors and does not necessarily represent the official view of the NIH. Dr Karmarkar is supported by a National Institutes of Health career development award no. K01-HD086290. Dr Krishnan is supported by a grant from the Agency for Healthcare Research and Quality (no. R24 HS022134) and National Institute of Disability, Independent Living and Rehabilitation Research (no. 90SFGE0002). The authors gratefully acknowledge the contributions of the study participants, their family members and caregivers, and all the research staff who participated in HEPESE. No borrowed material, copyrighted surveys, instruments, or tools were used for this article.
Author Information
Corresponding Author: Diane M. Collins, OT, PhD, University of Texas Medical Branch, Department of Occupational Therapy, 301 University Blvd, 3.916 School of Health Professions, Galveston, TX 77555-1142. Telephone: 409-772-3080. Email: dicollin@utmb.edu.
Author Affiliations: 1Department of Occupational Therapy, University of Texas Medical Branch, Galveston, Texas. 2Division of Rehabilitation Sciences, University of Texas Medical Branch, Galveston, Texas. 3Department of Health Services, Policy, and Practice, Brown University, Providence, Rhode Island. 4Division of Physical Therapy, Department of Rehabilitation Medicine, Emory University, Atlanta, Georgia. 5Department of Preventive Medicine and Community Health, University of Texas Medical Branch, Galveston, Texas.
References
- Administration on Aging. A statistical profile of Hispanic older Americans aged 65+. Washington (DC): Administration on Aging; 2014.
- Ortman JM, Velkoff VA, Hogan H. An aging nation: the older population in the United States. Current Population Reports. Washington (DC): US Census Bureau; 2014. p. 25-1140.
- US Census Bureau. The Hispanic population: 2010. Washington (DC): US Census Bureau; 2011. http://www.census.gov/prod/cen2010/briefs/c2010br-04.pdf. Accessed March 20, 2018.
- Health, United States, 2015: with special feature on racial and ethnic health disparities. Hyattsville (MD): National Center for Health Statistics; 2016. http://www.cdc.gov/nchs/data/hus/hus15.pdf. Accessed March 20, 2018.
- Samper-Ternent R, Kuo YF, Ray LA, Ottenbacher KJ, Markides KS, Al Snih S. Prevalence of health conditions and predictors of mortality in oldest old Mexican Americans and non-Hispanic whites. J Am Med Dir Assoc 2012;13(3):254–9. CrossRef PubMed
- Markides KS, Coreil J. The health of Hispanics in the southwestern United States: an epidemiologic paradox. Public Health Rep 1986;101(3):253–65. PubMed
- Sorlie PD, Backlund MS, Johnson NJ, Rogat F. Mortality by Hispanic status in the United States. JAMA 1993;270:2466–8.
- Marin G, Marin BV. Research with Hispanic populations. Newbury Park (CA): Sage Publications; 1991.
- Angel RJ, Angel JL, Hill TD. Longer lives, sicker lives? Increased longevity and extended disability among Mexican-origin elders. J Gerontol B Psychol Sci Soc Sci 2015;70(4):639–49. CrossRefPubMed
- Crist JD, Koerner KM, Hepworth JT, Pasvogel A, Marshall CA, Cruz TP, et al. Differences in transitional care provided to Mexican American and non-Hispanic white older adults. J Transcult Nurs 2017;28(2):159–67. PubMed
- Thomeer MB, Mudrazija S, Angel JL. How do race and Hispanic ethnicity affect nursing home admission? Evidence from the Health and Retirement Study. J Gerontol B Psychol Sci Soc Sci 2015;70(4):628–38. CrossRef PubMed
- Jindai K, Nielson CM, Vorderstrasse BA, Quiñones AR. Multimorbidity and functional limitations among adults 65 or older, NHANES 2005–2012. Prev Chronic Dis 2016;13:160174.CrossRef PubMed
- Whitson HE, Johnson KS, Sloane R, Cigolle CT, Pieper CF, Landerman L, et al. Identifying patterns of multimorbidity in older Americans: application of latent class analysis. J Am Geriatr Soc 2016;64(8):1668–73. CrossRef PubMed
- Prados-Torres A, Calderón-Larrañaga A, Hancco-Saavedra J, Poblador-Plou B, van den Akker M. Multimorbidity patterns: a systematic review. J Clin Epidemiol 2014;67(3):254–66.CrossRef PubMed
- Garin N, Koyanagi A, Chatterji S, Tyrovolas S, Olaya B, Leonardi M, et al. Global multimorbidity patterns: a cross-sectional, population-based, multi-country study. J Gerontol A Biol Sci Med Sci 2016;71(2):205–14. CrossRef PubMed
- Goodman RA, Ling SM, Briss PA, Parrish RG, Salive ME, Finke BS. Multimorbidity patterns in the United States: implications for research and clinical practice. J Gerontol A Biol Sci Med Sci 2016;71(2):215–20. CrossRef PubMed
- Bobo WV, Yawn BP, St Sauver JL, Grossardt BR, Boyd CM, Rocca WA. Prevalence of combined somatic and mental health multimorbidity: patterns by age, sex, and race/ethnicity. J Gerontol A Biol Sci Med Sci 2016;71(11):1483–91. CrossRef PubMed
- Quiñones AR, Markwardt S, Botoseneanu A. Multimorbidity combinations and disability in older adults. J Gerontol A Biol Sci Med Sci 2016;71(6):823–30. CrossRef PubMed
- Quinones AR, Markwardt S, Thielke S, Rostant O, Vasquez E, Botoseneanu A. Prospective disability in different combinations of somatic and mental multimorbidity. J Gerontol A Biol Sci Med Sci 2018;73(2):204–10. PubMed
- Markides KS, Rudkin L, Angel RJ, Espino DV. Health status of Hispanic elderly. In: Martin LG, Soldo BJ, editors. Racial and ethnic differences in the health of older Americans. Washington (DC): National Academies Press; 1997. p. 285-300.
- Rote S, Angel JL, Markides K. Health of elderly Mexican American adults and family caregiver distress. Res Aging 2015;37(3):306–31. CrossRef PubMed
- Radloff LS. The CES-D Scale: a self-report depression scale for research in the general population. Applied Psychological Measurement 1977;1(3 Summer):385-401.
- Folstein MF, Folstein SE, McHugh PR. “Mini-mental state.” A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975;12(3):189–98. CrossRefPubMed
- Ward BW, Schiller JS. Prevalence of multiple chronic conditions among US adults: estimates from the National Health Interview Survey, 2010. Prev Chronic Dis 2013;10:120203. CrossRefPubMed
- Buttorff C, Ruder T, Bauman ME. Multiple chronic conditions in the United States. Santa Monica (CA): RAND Corporation; 2017.
- Ashman JJ, Beresovsky V. Multiple chronic conditions among US adults who visited physician offices: data from the National Ambulatory Medical Care Survey, 2009. Prev Chronic Dis 2013;10:120308. CrossRef PubMed
- R Core Team: a language and environment for statistical computing. Vienna (AT): R Foundation for Statistical Computing; 2014.
- Goodman RA, Posner SF, Huang ES, Parekh AK, Koh HK. Defining and measuring chronic conditions: imperatives for research, policy, program, and practice. Prev Chronic Dis 2013;10:120239.CrossRef PubMed
- Steiner CA, Friedman B. Hospital utilization, costs, and mortality for adults with multiple chronic conditions, Nationwide Inpatient Sample, 2009. Prev Chronic Dis 2013;10:120292.CrossRef PubMed
- Bakas T, Pressler SJ, Johnson EA, Nauser JA, Shaneyfelt T. Family caregiving in heart failure. Nurs Res 2006;55(3):180–8. CrossRef PubMed
- Buchman AS, Boyle PA, Leurgans SE, Barnes LL, Bennett DA. Cognitive function is associated with the development of mobility impairments in community-dwelling elders. Am J Geriatr Psychiatry 2011;19(6):571–80. CrossRef PubMed
- McGough E, McCurry S, Logsdon R, Pike K, Teri L. Cognitive function and mobility disability in older adults with anmestic mild cognitive impairment. Alzheimers Dement 2012;8(4):P2–315.CrossRef
- Navaie-Waliser M, Feldman PH, Gould DA, Levine C, Kuerbis AN, Donelan K. The experiences and challenges of informal caregivers: common themes and differences among whites, blacks, and Hispanics. Gerontologist 2001;41(6):733–41. CrossRef PubMed
- Herrera AP, Mendez-Luck CA, Crist JD, Smith ML, Warre R, Ory MG, et al. Psychosocial and cognitive health differences by caregiver status among older Mexican Americans. Community Ment Health J 2013;49(1):61–72. CrossRef PubMed
- Hahn EA, Kim G, Chiriboga DA. Acculturation and depressive symptoms among Mexican American elders new to the caregiving role: results from the Hispanic-EPESE. J Aging Health 2011;23(3):417–32. CrossRef PubMed
































No hay comentarios:
Publicar un comentario